|
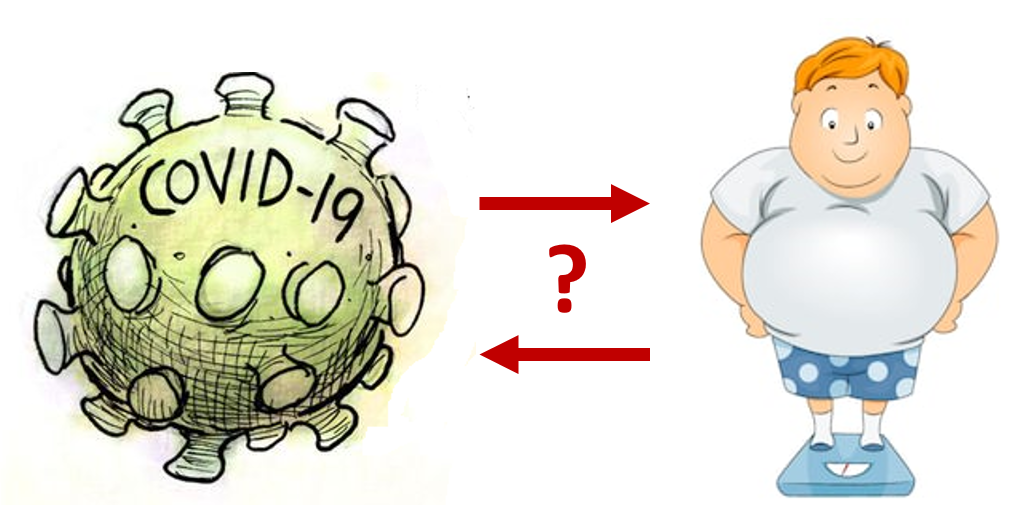
In the short time since the novel coronavirus COVID19 has taken the U.S. by storm, more than 80% of Americans are now waking up to a “new normal” in which we cannot go to work or school outside our home. If we do venture out, we are advised to wear cloth masks and stay at least six feet away from others. Amidst these major changes to our daily lives, I’ve been noticing friends and coworkers grumble about how they won’t be able to fit into their work clothes when this all ends since they can’t go to the gym. “Instead of the Freshman 15, we will gain the COVID 19,” my mother-in-law joked. While this is potentially true (and rather unfortunate), I have been more preoccupied with another relationship between the virus and excess weight: it appears as though persons with overweight or obesity are more likely to suffer complications of COVID19, even if they are otherwise healthy. At the beginning, the only evidence I came upon was anecdotal. I heard from a colleague who works in the ER that a 33-year-old is on a ventilator. “He’s healthy,” she said, “and doesn’t smoke. No history of asthma, bronchitis, or any other medical complications… oh, but he is overweight.” As my curiosity grew, I began scouring the internet and realized that because the pandemic evolved so quickly, the articles I came across could only allude to data that had not yet been published (e.g., this article in the New York Times). Just this week, I found a hot-off-the-press paper published in Clinical Infectious Diseases. (Note that this paper was published and made available so swiftly that the hyperlink takes you to a PDF manuscript draft rather than a polished galley proof formatted for a journal.) In this retrospective registry-based analysis of 3,615 individuals who presented to a large academic hospital in New York City and tested positive for COVID19, the authors found higher risk of complications (defined as requiring intensive care accommodations or a ventilator) among patients <60 years of age with obesity. Despite coming up relatively short-handed on hard evidence (i.e., just one published paper showcasing simple unadjusted associations to support my hypothesis), I am relieved to see peer-reviewed research trickling through on this topic, especially since there are some plausible biological explanations regarding why excess weight would make COVID19 worse:
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
©2017 WeighingInBlog. All rights reserved. 401 Park Drive, Boston, MA




 RSS Feed
RSS Feed

