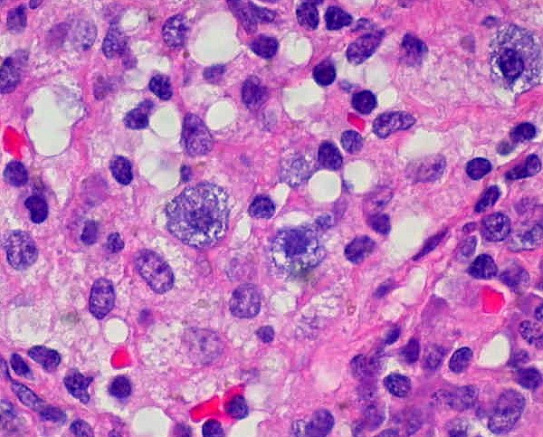
 What feels like a food allergy, looks like a food allergy, but is NOT actually an allergy? The answer for me was mast cell activation syndrome, or MCAS. Two years ago, I marched myself to the doctor, convinced that I had an undiagnosed food allergy. I explained my symptoms—chronic hives and itching, intense facial flushing, gastrointestinal upset, headaches, and difficulty breathing out of my nose, especially after eating. After much discussion about my symptoms and medical history, my amazing allergist realized my symptoms for what they were—a mast cell disorder. I was diagnosed with mast cell activation syndrome; a newly recognized immune system disorder that normally takes an average of 10 years to accurately diagnose. Although MCAS is currently quite rare, experts estimate that it is actually very common, with many cases going undiagnosed. MCAS was first recognized in 1991, and only named and assigned diagnostic criteria in 2007. MCAS is characterized by overactive mast cells, which are part of the immune system. Among other things, mast cells contain histamines; during an allergic reaction, the cells are triggered and release histamines into the surrounding tissues, causing itching and irritation. In MCAS, because the mast cells are overactive, histamine builds up in the body and causes people with MCAS to feel like they are constantly having an allergic reaction. There are a lot of mast cells in the skin (hence the flushing, itching, and hives I experience), but there are also mast cells in your gastrointestinal tract, within your nasal passages, and elsewhere in your body, causing irritation and upset across the board.
So what can people with MCAS do to treat their condition? Besides taking antihistamines like Zyrtec, those with MCAS are advised to adopt a low-histamine diet . Yes, foods have varying levels of histamine. Eating too many high-histamine foods causes overactive mast cells to go into overdrive, creating the uncomfortable reactions described above. So what does the diet entail? Since histamine levels increase as food ages and bacteria levels increase, a low-histamine diet generally means no leftovers, foods that are heavily processed or contain artificial additives, and aged or fermented foods. Fresh and freshly prepared foods usually have lower levels of histamines. This makes going out to eat, grabbing snacks, and sharing food difficult, but I find that it also leads to a healthier way of eating. After adopting my version of the low-histamine diet—I try to eliminate or eat less high-histamine “junk” food and eat more antihistamine, high-nutrient food, a la The Low Histamine Chef— my MCAS is better controlled, and I am much happier. Food, once my enemy, has helped heal me both physically and mentally. Pretty cool stuff.
1 Comment
Angie Thrower
10/1/2015 05:12:13 am
Thank you for posting Mia!! I have a friend struggling with similar symptoms and have passed this along.
Reply
Your comment will be posted after it is approved.
Leave a Reply. |
©2017 WeighingInBlog. All rights reserved. 401 Park Drive, Boston, MA



 RSS Feed
RSS Feed

